DIGITAL PATIENT CARE ASSIST (DPCA)
A suite of tools for assisting individuals who deal with chronic and long-term morbidity conditions.
Overview
Problem: Chronic and long-term diseases are prevalent among Canadians. Patients face many challenges and frustrations, especially people suffering from more than one long-term condition. On the other hand, dealing with all of the health instructions from multiple health care professionals is a challenge for both the patient and the patient’s healthcare team.
Target users: It targets individuals who suffer from chronic and multimorbidity conditions.
Goal: The goal is to create genuine and effective solutions, in an integrated healthcare system to empower patients and improve their healthcare outcomes.
Objectives: Leverage AI & Machine learning for a patient-centered care assist service that collects and demonstrates health data and offers plans and recommendations to patients. This information and extracted insights are not only beneficial for patients, but also facilitate interactions between different health care professionals from each patient’s healthcare team.
My Role: I led the project, from research and ideation to development of the Hi-Fi prototype. This is an ongoing project, currently we are in the user testing phase. So far, I've been utilizing the following methods and tools:
-> Secondary research
-> Survey
-> Interview
-> Affinity Map
-> Journey Map
-> Storyboard
-> User flow
-> Wireframing (Low & high fid)
-> Usability testing
-> Illustrator & XD
-> Whimsical
-> Miro
-> UX Pressia
Client - ISM Arts and Culture
Research Context
Problem Space
In Canada, it’s an unfortunate fact that few people are untouched by chronic diseases. In fact, three out of five people over the age of twenty live with one or more non-communicable chronic diseases(Government of Canada, 2018). According to Public Agency of Canada, 73% of individuals aged 65+ and 44% of adults aged 20+ years have at least 1 of 10 common chronic diseases. (Public Health Agency of Canada, 2020)
Individuals with chronic conditions and multimorbidity experience many challenges and frustrations in the management of their conditions. Multimorbidity is the occurrence of two or more long-term conditions. According to C3-Cloud, a European union funded research project in personalized care, finding the best way to support and treat people with multimorbidity, can be extremely challenging. Dealing with all of the health instructions from multiple health care professionals is a challenge both for patients and the healthcare teams.
A fundamental shift from disease-centered to patient-centered
What is a patient-centered approach?
In terms of self management, lack of required skills and knowledge in patients and other gaps in disease-centered health care services cause frustrations, longer treatment periods and in some cases unsuccessful treatments for patients. However, In a patient-centered healthcare system there is cooperation amongst all actors with a focus on the patient. It requires information to be integrated so that across the entire range of actors, support is efficiently and effectively provided to patients to enable them to play a bigger role in their own health and wellness.(Person-Centered Care, n.d.)
Chronic disease requires a fundamental shift from disease-centered approach to patient- and family-centered approach, combining self-management in the community with well-integrated professional support through the life-course (EPF Background Brief: Patient Empowerment, n.d.). Engaging patients in the medical journey plays an essential role in the success of the treatment. Studies have shown that activated patients have better health outcomes and better care experiences than patients who are less activated(Challenges | C3-Cloud, n.d.). According to the study on teenagers with chronic arthritis at BC children’s hospital, involving teenagers and their caregivers in pain management may help them become more engaged in their care, follow the chosen treatments, manage their disease better, and lead to better health outcomes. (Chronic Pain Network | Home, n.d.)
Affinity Diagram from Patient Concerns
I gathered valuable information regarding the problems and pain points in patients' medical journeys from the user interviews and surveys. I clustered and organized them into the below categories that helped me to understand and find the underlying problems.
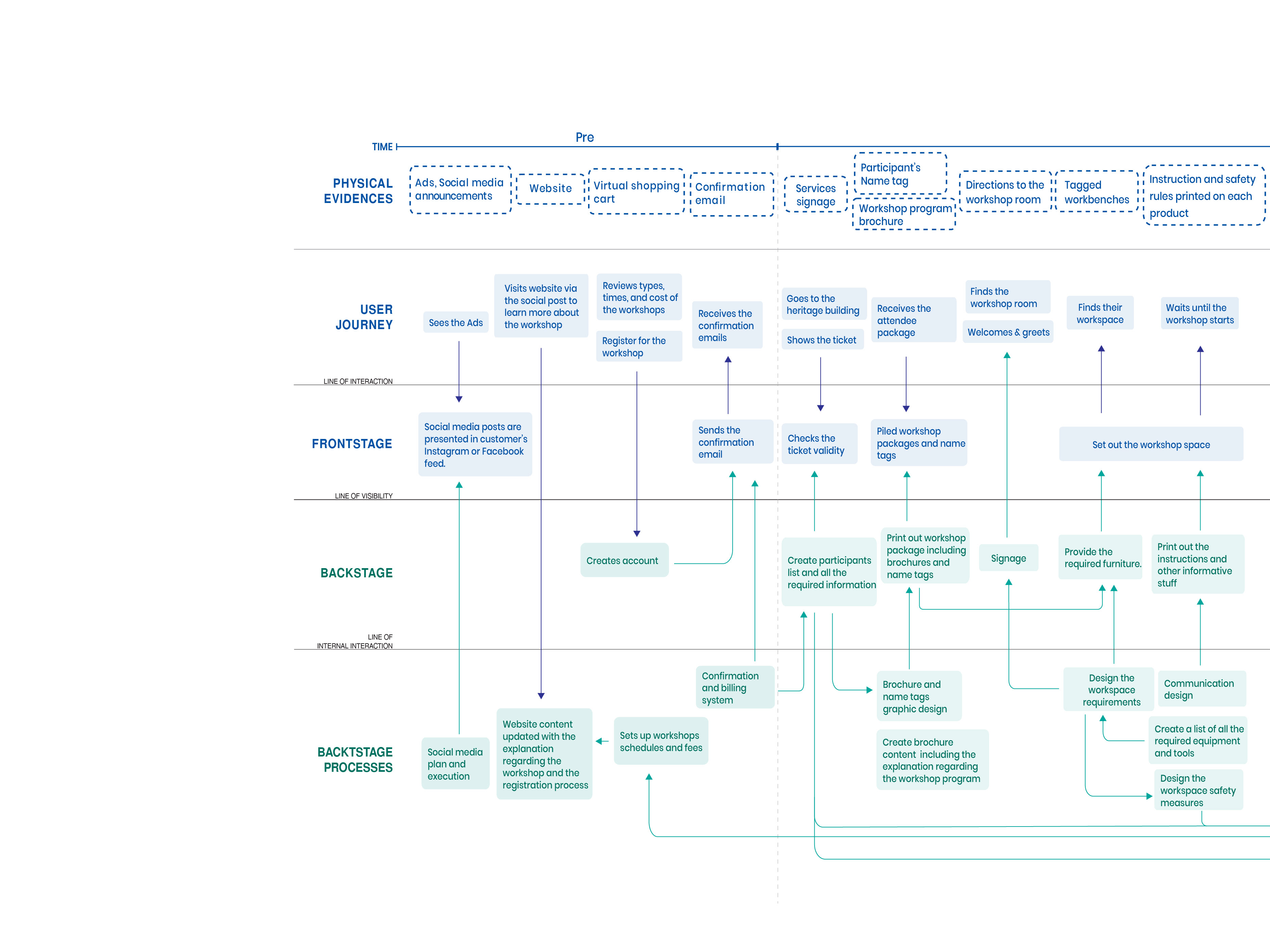
Experience Journey Map
Ethnographic Research Findings
Key frustrations found in a medical journey both for patients and healthcare team
Challenge – Depending on the type of treatment instructions, patients might not practice their exercises properly. In this regard, one of the physiotherapists confirmed that some patients participate well, while some do not cooperate, and we can not force them to act differently.
Solution - Involving patients in the treatment process, helps to inspire the patients to cooperate actively. The way and pace at which patients do the treatments could be shared with their healthcare professionals. Furthermore, both the patients and the healthcare team could be able to communicate with each other on the platform. (E.g., text messages, email, video call, etc.)
Challenge – Patients might forget or lose the treatment instructions either in a physical or e-document format. After a while, archiving documents becomes a big task.
Solution - A platform that collects and organizes everything that health practitioners prescribe and suggests to patients.
Challenge – In some cases, health instructions have to become a part of an individual's lifestyle. Thus, patients need to be supported to adopt new habits.
Solution - Artificial intelligence could assist patients and their caregivers by planning, strategizing, and reminding them to do their daily practices.
Challenge – In some long-term and morbidity treatments, progress happens gradually and slowly. The patient might find the treatment process very repetitive, boring, and they might even be unable to see the small improvements. So, this could stop them from healing properly since they might get used to the discomfort and never fully treat it.
Solution - Demonstrating the medical journey milestones in understandable formats.
Challenge – In some cases, patients do not have enough knowledge about their disease or they are curious to know more about it. In these situations, the first thing that they do is search online. However, there are thousands of various, unrelated, and unreliable resources which could overwhelm and misinform people regarding a serious condition.
Solution - Patients need to be informed how to access the reliable resources. Artificial intelligence could be used to educate them with relevant topics. In addition, healthcare professionals and caregivers could share the related and persuasive articles with their patients.
Challenge – Sometimes treatments might not be as effective as a health professional expects them to be.
Solution - Based on the collected info, the healthcare team could assess how each treatment instruction has affected the problem. (Dashboard report)
Challenge – The same instructions and treatments might not have the same impact on every patient with similar symptoms.
Solution - An integrated system that offers personalized planning and strategies. (i.e., with a holistic approach, considering other simultaneous treatments, vital signs, lifestyle habits, etc.)
Challenge – Some treatment instructions are not covered under governmental insurance and extended health care coverage is usually limited. (e.g., physical therapies)
Solution - In situations that an in-person visit is not necessary, people could still benefit from many other services that would be relatively inexpensive.
Expert Interview results
While healthcare interviewees are genuinely concerned how reliable an AI planner and diagnosis could be, they believe that incorporating the following requirements must be considered in designing a reliable planning and diagnosis system.
From interviews with physicians, specialists, and other healthcare practitioners such as physical and occupational therapists, we concluded that in term of the types of visits between healthcare team and patients there are two main categories:
1- Unnecessary in-person check up/follow up.
There are situations like increasing medication dosage, referral request and/or following up an ongoing situation.
2- Necessary in-person check up.
In some severe conditions, patients are not conscious enough to be aware of all their symptoms therefore there has to be an in-person check-up. Accordingly, one of the psychiatrists explained that, for example if a patient has a severe headache, might not be able to realize eyelid twitching. In this case and similar situations in-person visits are required to do physical and reflex tests.
Design Approach
Research shows that there are many factors that play into the patient experience during a medical journey. We believe that providing tools and tweaking the patient’s interactions in each part of the health care system will lead to a better experience both for patients and health care providers. In designing this tool, we have been attempting to address the existing challenges with an empowerment and patient-centered approach. According to the European Patients Forum(EPF), the five “Es” of Empowerment are Education, Expertise, Equality, Experience, and Engagement.
1. Educate - Patients can make informed decisions about their health if they are able to access all the relevant information, in an easily understandable format.
2. Expertise - To assist patients in self-managing treatment. Patients self-manage their condition every day so they have a unique expertise on their healthcare journey which needs to be supported
3. Equality - Patients need support to become equal partners with health professionals in the management of their condition.
4. Experience - Individual patients work with patient organizations to represent them, and channel their experience and collective voice.
5. Engage - Engage patients in the treatment process. Patients need to be involved in designing more effective healthcare for everyone's benefit and in need to play a role research to deliver new and better treatments and services.
Product Features
Mobile app sitemap
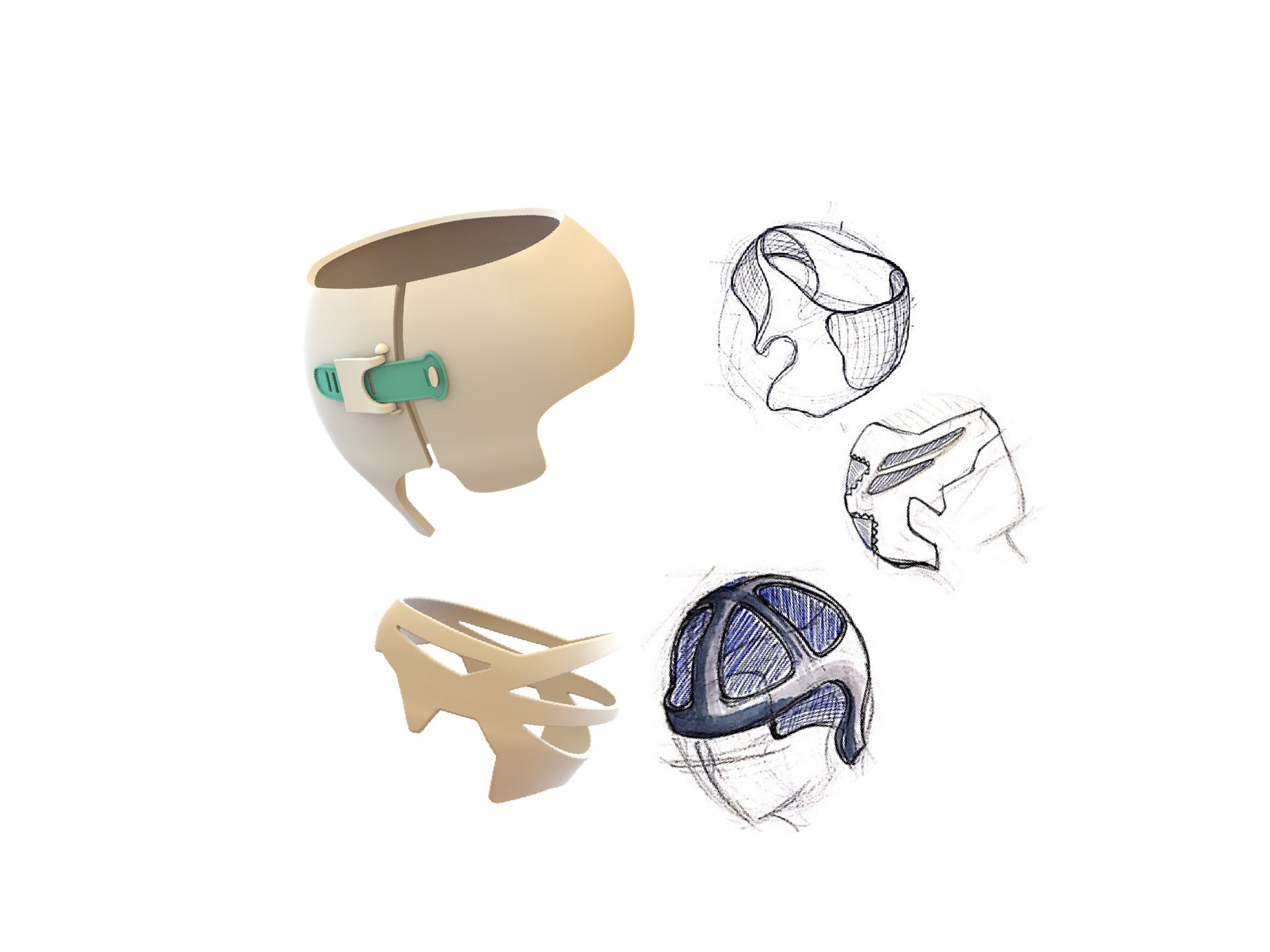
Wireframes
Low & High Fidelity Prototypes
Reflections
- I really enjoyed leading this project from scratch to implementation. Conducting surveys and interviews with patients and the healthcare providers were very helpful and gave me a deep understanding of the problem context.
- DPCA tools are meant to facilitate the treatment journey both for patients and the healthcare providers and should not be considered as substitutes for professional diagnosis such as visiting a doctor.
- Keeping confidential patient data safe and secure is an essential part of digital healthcare services. Therefore, data security solutions should be incorporated in running such a service.
- In order to ensure that the product is 100% inclusive I’d like to test the tools on a wider range of participants. In addition, for the demography of Canada this service should be available in multiple languages.
Stay tuned as this project progresses! Contact me if you have any questions!